Findings are a promising step toward developing improved treatments for the disease
UCLA researchers have identified mechanisms that determine how advanced melanoma can become resistant to immune checkpoint inhibitors, a discovery that could lead to the development of new and improved treatments for the deadliest type of skin cancer.
Immunotherapy using the anti-PD-1 antibody pembrolizumab (marketed as Keytruda) has revolutionized the treatment of advanced melanoma. But a minority of patients who respond to treatment still experience reappearance and progression of their tumors, said Dr. Antoni Ribas, director of the UCLA Jonsson Comprehensive Cancer Center Tumor Immunology Program.
“The tremendous promise of immunotherapy is to engage our body’s immune defenses to fight cancer, but the results must be long-lasting,” said Ribas, professor of hematology and oncology at UCLA. “We have now identified for the first time mechanisms that cancer cells can use to avoid recognition by the immune system’s T cells and decrease sensitivity to their attack.”
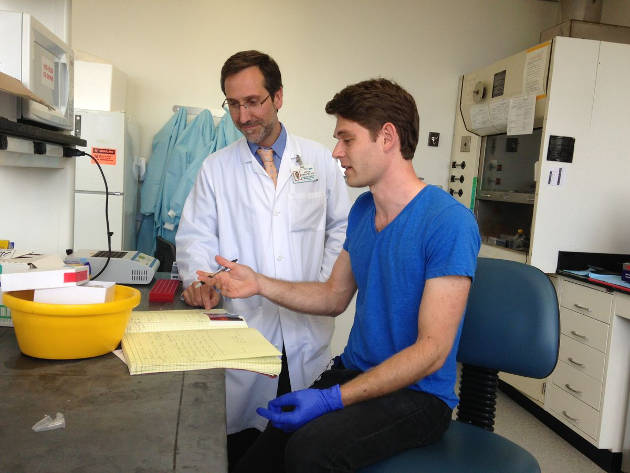
Dr. Antoni Ribas (left) with lab team member and study first author Jesse Zaretsky. Photo credit: UCLA Jonsson Comprehensive Cancer Center
The study is published online in the New England Journal of Medicine.
The researchers analyzed biopsies of melanoma tumors from patients that received pembrolizumab. The team compared pairs of tumors, both before the patients started treatment and after relapse, which occurred several months to years later. Among the four pairs of biopsies studied, the team found one tumor lost a gene called B2M, resulting in a change in how the cancer is recognized by the immune system. Two additional tumors developed defects that disrupted the function of genes JAK1 or JAK2, which limited the effectiveness of the immune system to kill cancer cells.
*Source: University of California
