Human Papillomavirus (HPV) drives a greater number of head and neck cancers than previously thought, finds new research from UCL and the University of Southampton.
The findings, published in the Journal of Clinical Oncology, offer valuable insight into the role of HPV in tumour development and explore the possibility of a viable treatment option for specific cancer patients.
HPV affects the skin and the moist membranes that line parts of the body. There are over 100 different types of the virus and the body’s immune system is normally able to get rid of an HPV infection without it causing any problems. However,some HPV types are known to cause specific cancers, in particular cervical cancer and tonsil cancers (oropharyngeal cancers).
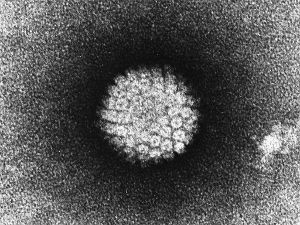
Human Papillomavirus (Image courtesy of Wikimedia Commons)
It is known that in HPV associated (HPV+) oropharyngeal cancer, there’s a very strong link between the number of immune cells (T-cells) in the tumour and patient survival – when high numbers of T-cells are present, patients respond well to therapy (either surgery or chemoradiotherpay). When tumours are not caused by the virus (HPV-), far fewer immune cells are present, and patients do not respond as well to treatment. This suggests that the cancers caused by virus are more readily detected by the patients’ immune systems, and this intrinsic immune response plays a key role in the better survival of most patients with HPV+ cancers.
So, when the team discovered that HPV was also driving a small percentage of head and neck cancers at sites other than the oropharynx, it seemed likely that these patients would also experience significantly better survival rates. Surprisingly this was not the case.
“When we looked at HPV+ cancers at other head and neck sites, we didn’t see the same survival benefit or infiltration of T-cells as we did in the HPV+ tonsil cancers.” explains Dr Tim Fenton, Senior Research Associate, UCL Cancer Institute, and senior author of the study. “And we think that this is the major difference in determining the difference in patient prognosis.”
So why is there such a marked difference in immune cell numbers in HPV+ oropharyngeal cancer and HPV+ cancers at other sites in the head and neck? The answer may lie in the anatomy of the oropharynx (tonsils).
Dr Fenton says “The tonsils are composed of lymphoid tissue, so there are many immune cells already present in this area. There’s a possibility that cancers developing in the tonsils are very visible to the immune system in that respect. However, HPV- oropharyngeal cancers contain far fewer T-cells, so it appears to be a combination of having a virally driven cancer that is located in the tonsil that gives a strong immune response, and much better clinical outcome.”
“The other important point to take from this study, is that there are HPV-targeted therapeutic vaccines in clinical trials at the moment. In fact the Southampton team are about to open a clinical trial testing one such vaccine (HARE-40 Trial) . Currently, we test oropharyngeal cancers for HPV, but not cancers arising at other sites in the head and neck. Even though numbers of these patients are relatively small – approximately 1 in 25 patients – the likely benefit from vaccination, particularly as these treatments become more fully developed, means that testing should be more widespread for these specific cancers”
Research was funded by the Rosetrees Trust, CRUK. Ankur Chakravarthy was the recipient of UCL Graduate Research School and Overseas Research Scholarships
*Source: University College London
