Early-warning sensor systems that can test and track serious infectious diseases – such as major flu epidemics, MRSA and HIV – using mobile phones and the internet are being developed by a major new Interdisciplinary Research Collaboration (IRC) led by UCL.
The new £11 million IRC, funded by the Engineering and Physical Sciences Research Council (total investment £16 million), will develop mobile health technologies that allow doctors to diagnose and track diseases much earlier than ever before.
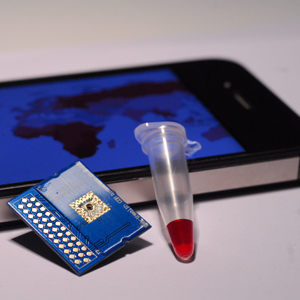
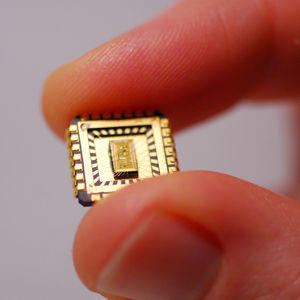
The IRC will pioneer low cost, easy to use mobile phone-connected diagnostic tests based on advances in nanotechnology for use in GP surgeries, pharmacies, elderly care homes, developing countries and at home.
The mobile tests aim to identify diseases with high sensitivity and specificity and give results within minutes from just a pin-prick of blood or a simple swab. Rapidly transmitting results into secure healthcare systems will alert doctors to potentially serious outbreaks with geographically linked information.
The IRC brings together scientists, engineers and clinicians from UCL, Imperial College, the London School of Hygiene and Tropical Medicine and Newcastle University, together with NHS stakeholders UCL Partners, Newcastle Hospitals NHS Foundation Trust, the NIHR University College London Hospitals Biomedical Research Centre, the NIHR Newcastle Biomedical Research Centre, Public Health England and industry partners – OJ-Bio, Microsoft, Cambridge Life Sciences, Mologic, O2 Health, Zurich Instruments, XFAB and Cepheid.
The UCL team are already developing a smart-phone-connected prototype test for HIV with industry partners OJ-Bio.
The IRC will also track reported symptoms of infection by searching millions of internet sources including media reports, search engine queries (e.g. Google Trends and Bing) and social networking sites (e.g. Facebook and Twitter) to identify outbreaks even before people attend clinics or from parts of the world that lack the resources for traditional public health surveillance.
Worldwide, there are an estimated 6.8 billion mobile phone subscriptions, 2.7 billion people on-line and 1 billion social network users, representing a massive opportunity to widen access to tests and track emerging disease outbreaks.
Dr Rachel McKendry, from the London Centre for Nanotechnology UCL, who will lead the new centre, said: “A new generation of diagnostic test and tracking systems could save millions of people from deadly diseases such as new strains of influenza, HIV and MRSA.”
“The revolution in mobile communication, nanotechnology, genomics, and ‘big data’ analysis offers tremendous opportunities to actively manage outbreaks and ultimately prevent infectious diseases. Widening access to tests in community settings will empower patients to gain faster access to treatment, reduce the inappropriate use of antibiotics and protect the wider public.”
The new centre will bring critical mass and multidisciplinary expertise in biomarker discovery (“pathogen-specific fingerprints”) which require minimal sample processing steps, nano-enabled sensors, temperature-stable biomimetic capture coatings, nanoparticles, microelectronics, microfluidics, wireless networks, data mining, data security and health economics.
Early diagnosis plays a vital role in the treatment, care and prevention of infectious diseases. However, worldwide, many infections remain undiagnosed and untreated or are diagnosed at the late stage due to poor diagnostic tools. The result is on-going transmission of serious infections and delays in the identification of emerging threats.
Professor Deenan Pillay, Infectious Diseases Programme Director for the NIHR University College London Hospitals Biomedical Research Centre, and clinical lead of the new EPSRC IRC said: “Infectious diseases remain among the top killers in the world. Newly emerging pandemics of, influenza, for example, provide major threats, and the spread of infections within hospitals and communities often undermines our effective management of patients, whatever their health problems.
“One of the major limitations to effective prevention, treatment and cure is the lack of appropriate tools to diagnose infections in the first place and monitor effective treatment.”
To meet the needs of end users, the team will work closely with leading NHS clinicians from UCL Partners, Newcastle NHS Trusts, NIHR Biomedical Research Centres, Public Health England, patient groups and the public to address the wider issues of increased testing, care pathways and data security. The centre also benefits from links to more than 100 countries in Africa, Asia and South America via the LSHTM International Diagnostics Centre led by Professor Rosanna Peeling.
Professor Calum McNeil, lead investigator from Newcastle University said, “For me the EPSRC IRC is a long-term ambition come true. It presents a fantastic opportunity to work with world-leaders in nanotechnology, engineering, bioinformatics and communications technologies in order to provide real-time predictive, preventive, point-of-care healthcare provision – a hugely exciting undertaking.”
Two other healthcare IRCs are being funded by EPSRC as part of a £32m funding award. Welcoming the centres, David Willetts, Minister for Universities and Science, said: “New British technologies are transforming healthcare and saving lives, for example, in future, our smart phones will tell us when we are ill, controlling the spread of infectious diseases. As healthcare challenges become more complex, our world-class scientists are finding the next generation solutions.”
*Source: University College London